End-to-end IT solutions for healthcare organizations.
Fix Your Revenue Cycle at the Source.
We fix broken billing workflows, optimize EHRs, automate eligibility verification, and improve clean claim rates — so your practice can get paid faster and stay compliant

Are These Revenue Cycle Pain Points Slowing You Down?
End-to-End RCM Support for Mid-Sized Practices
Medical practices often struggle with cash flow and operational inefficiencies that start at the front desk and echo through the entire revenue cycle. If any of the following sounds familiar, you're not alone — and we can help.
-
Preventable coding errors, outdated payer rules, and poor follow-up lead to costly delays and write-offs.
-
Manual denial management and limited prioritization of aged claims reduce revenue.
-
Incomplete eligibility checks and disconnected scheduling tools cause no-shows and billing issues.
-
Manual intake processes introduce errors before the patient even sees the provider.
-
EMRs, billing, and CRM platforms that don’t “talk” to each other force staff to duplicate efforts.
-
Legacy systems limit automation, analytics, and flexibility, creating a drag on productivity.
-
Billing teams are overwhelmed or undertrained.
-
High turnover leads to inconsistencies in coding, claims management, and payer communication.
-
You can’t manage what you can’t measure. Limited dashboards make it hard to track denial trends, A/R aging, and net collection rates.
-
Difficult to forecast revenue, spot leakage, or measure performance.
-
Struggles meeting MIPS, MACRA, and other regulatory requirements while avoiding penalties.
-
Challenges aligning clinical and financial workflows and tracking quality metrics tied to reimbursement.
Let’s Fix What’s Holding You Back
At Provisions Group, we don’t just diagnose the problems in your revenue cycle — we fix them. Our team combines deep healthcare operations experience with technical know-how to resolve root issues inside your EHR and workflows — where the real problems live.
How We Help Practices Like Yours

-
Redesign scheduling, intake, and eligibility workflows
-
Implement best practices for denial management, A/R recovery
-
Improve first-pass claim rates and payer communication

- Configure charge capture, documentation templates, and CPT code mappings
- Align clinical and billing workflows inside Epic, Athena, Greenway, and others
- Eliminate issues that cause denials at the point-of-care

- Connect your EMR, billing, CRM, and patient engagement tools
- Automate eligibility checks, claims processing, and financial reporting

- Provide interim or long-term experts in billing, coding, analytics, IT, and RCM leadership
- Access niche expertise in payer contracting, denial management, and analytics

- Deploy dashboards for key KPIs: Days in A/R, denial rates, net collections, and more
- Turn your data into insights that drive action and improvement

- Support MIPS/MACRA strategy, documentation improvement, and reporting
- Align clinical workflows with quality metrics and reimbursement models
Let’s Talk About Your Revenue Cycle
Get Paid Faster With Hands-On RCM Execution. Ready to reduce A/R, improve reimbursements, and simplify your billing processes?
We Don’t Just Advise. We Fix What Others Can’t
Most RCM consultants leave you with a list of recommendations. We roll up our sleeves and make the changes directly inside your systems – eliminating the root causes of delays, denials, and missed revenue. Our team has the technical depth and healthcare experience to make real, lasting changes inside your systems, not just recommend them.
Improved Cashflow & Stronger Financial Performance
- Lower denial rates and faster reimbursements
- Improved cash flow and net collection through better charge capture and follow-up
- Reduce denials, speed up reimbursements, and improve net collection rates
Data-Driven Decisions
- Real-time dashboards and reporting to track key revenue cycle KPIs
- Actionable insights to identify revenue leakage and guide strategy, staffing, and investments
Operational Efficiency & EHR Optimization
- Streamlined scheduling, intake, and billing workflows
- Optimized EHR setup—charge capture, documentation templates, and payer rules – to reduce delays and denials
- Fewer manual tasks and smoother collaboration between clinical and financial teams
People & Long-Term Readiness
- Training and support that reduce burnout and turnover
- Confidence in compliance, value-based care, and audit readiness
- Scalable technology and workflows aligned with long-term growth
Still Not Sure Where to Start?
Let’s take a quick look at your workflows, denial trends, or EHR setup and show you exactly what’s blocking your cash flow.
Why Choose Provisions Group?
Hands-On Revenue Cycle Execution and EHR Expertise
We’re more than RCM consultants — we have deep, hands-on experience with leading EHR platforms and healthcare operations. We understand how clinical documentation, charge capture, billing workflows, and payer rules all interact. That means we don’t just identify revenue cycle issues — we go into your EHR and systems and fix them.
We understand that revenue cycle issues often stem from how your EHR is configured, not just how your teams are using it. That’s why we:
- Fix charge capture workflows, documentation templates, and payer rule setups
- Align clinical documentation with billing requirements
- Ensure your EHR supports clean claims and efficient scheduling








FEATURED SUCCESS STORY
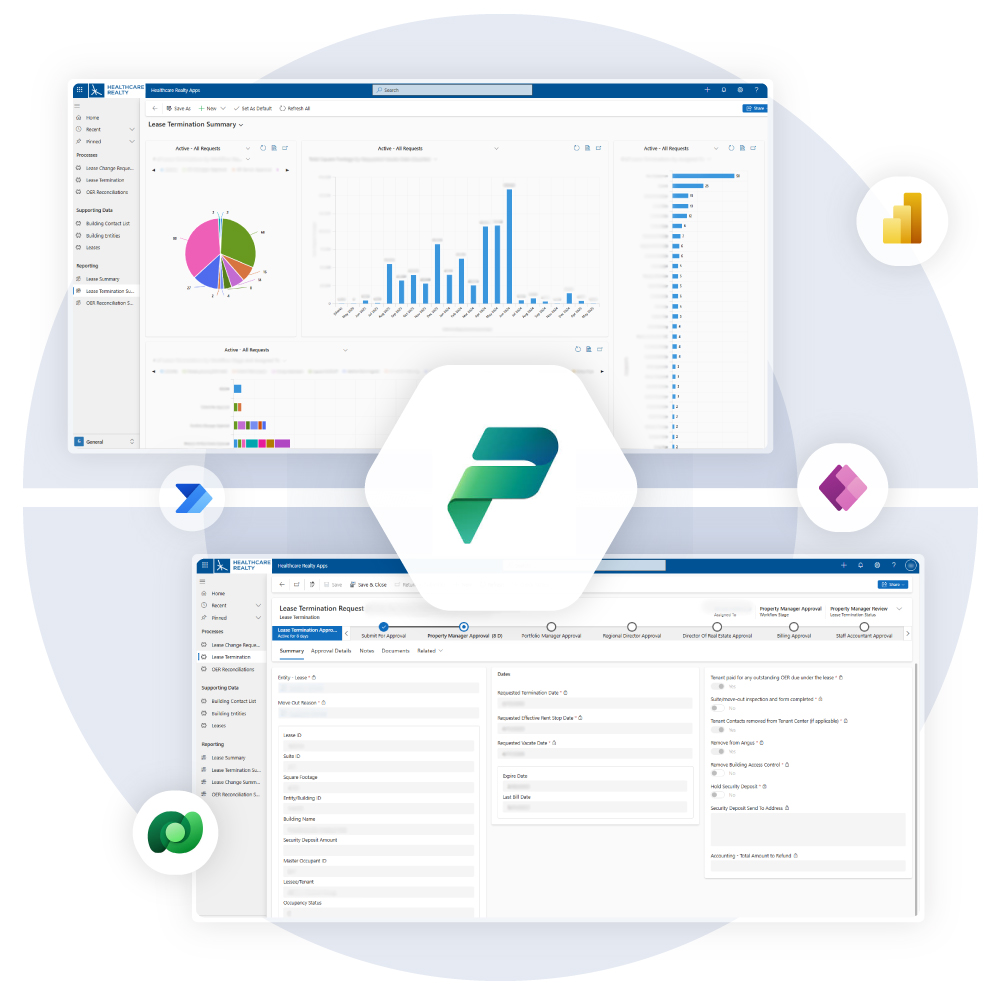
How we streamlined lease management tools and cut support tickets by 75%.
Healthcare Realty Trust, a publicly traded REIT specializing in outpatient medical facilities, partnered with Provisions Group to modernize their lease management processes. Using Microsoft Power Platform—including Power Apps, Power Automate, and Dataverse—we streamlined workflows, reduced support tickets by 75%, and improved cross-team collaboration across operations, leasing, and accounting.
Frequently Asked Questions
We address denials and A/R at the source:
- Fixing coding errors and updating payer rules inside your EHR.
- Redesigning denial management workflows.
- Automating claim follow-up and prioritization.
- Training staff on best practices to prevent future issues.
We streamline your front-end workflows by:
- Automating eligibility verification and scheduling.
- Reducing manual data entry errors during intake.
- Integrating scheduling tools with your EHR and billing systems to ensure clean claims from the start.
Clients typically see:
- Lower denial rates and A/R days.
- Increased cash flow and net collection rates.
- Streamlined workflows and EHR setup.
- Better compliance and confidence in audits.
Let's Fix Your Revenue Cycle.
Provisions Group brings together healthcare RCM specialists, EHR experts, and technical consultants to fix what’s broken and help your practice get paid — faster and more efficiently.
